- ANAL ABSCESS/FISTULA
- ANAL CANCER
- ANAL FECAL INCONTINENCE
- ANAL FISSURE
- ANAL WARTS
- COLONOSCOPY
- COLON RECTAL SURGERY
- COLORECTAL CANCER
- SERGERY-FOLLOW UP EVALUATION
- CONSTIPATION
- CROHN’S DISEASE
- DIVERTICULAR DISEASE
- GENETICS AND COLORECTAL CANCER
- HEMORRHOIDS
- IRRITABLE BOWEL SYNDROME
- OSTOMY
- PELVIC FLOOR DYSFUNCTION
- PILONIDAL DISEASE
- POLYPS OF THE COLON AND RECTUM
- PRURITUS ANI
- RECTAL PROLAPSE
- RECTOCELE
- SCREENING & SURVEILLANCE
- ULCERATIVE COLITIS
Anal Abscess/Fistula
Anal Abscess/Fistula
A patient who feels ill and complains of chills, fever and pain in the rectum or anus could be suffering from an anal abscess or fistula. These medical terms describe common ailments about which many people know little.
What is an anal abscess?
An anal abscess is an infected cavity filled with pus found near the anus or rectum.
What is an anal fistula?
An anal fistula is almost always the result of a previous abscess. Just inside the anus are small glands. When these glands get clogged, they may become infected and an abscess can develop. A fistula is a small tunnel that forms under the skin and connects a previously infected anal gland to the skin on the buttocks outside the anus.
 What causes an abscess?
What causes an abscess?
An abscess results from an acute infection of a small gland just inside the anus, when bacteria or foreign matter enters the tissue through the gland. Certain conditions – colitis or other inflammation of the intestine, for example – can sometimes make these infections more likely.
What causes a fistula?
After an abscess has been drained, a tunnel may persist connecting the anal gland from which the abscess arose to the skin. If this occurs, persistent drainage from the outside opening may indicate the persistence of this tunnel. If the outside opening of the tunnel heals, a recurrent abscess may develop.
What are the symptoms of an abscess or fistula?
An abscess is usually associated with symptoms of pain and swelling around the anus. Individuals may also experience fatigue, fevers and chills. Symptoms related to the fistula include irritation of the skin around the anus, drainage of pus (which often relieves the pain), fever, and feeling poorly in general.
Does an abscess always become a fistula?
No. A fistula develops in about 50 percent of all abscess cases, and there is really no way to predict if this will occur.
How is an abscess treated?
An abscess is treated by making an opening in the skin near the anus to drain the pus from the infected cavity and thereby relieve the pressure. Often, this can be done in the doctor’s office using a local anesthetic. A large or deep abscess may require hospitalization and the assistance of an anesthesiologist. Hospitalization may also be necessary for patients prone to more serious infections, such as diabetics or people with decreased immunity. Antibiotics are a poor alternative to draining the pus because antibiotics do not penetrate the fluid within an abscess.
What about treatment for a fistula?
Surgery is necessary to cure an anal fistula. Although fistula surgery is usually relatively straightforward, the potential for complication exists and is preferably performed by a specialist in colon and rectal surgery. It may be performed at the same time as the abscess surgery, although fistulas often develop four to six weeks after an abscess is drained, sometimes even months or years later.
Fistula surgery usually involves opening up the fistula tunnel. Often this will require cutting a small portion of the anal sphincter, the muscle that helps to control bowel movements. Joining the external and internal openings of the tunnel and converting it to a groove will then allow it to heal from the inside out. Most of the time, fistula surgery can be performed on an outpatient basis. Treatment of a deep or extensive fistula may require a short hospital stay.
How long does it take before patients feel better?
Discomfort after fistula surgery can be mild to moderate for the first week and can be controlled with pain pills. The amount of time lost from work or school is usually minimal.
Treatment of an abscess or fistula is followed by a period of time at home when soaking the affected area in warm water (sitz bath) is recommended three or four times a day. Stool softeners or a bulk fiber laxative may also be recommended. It may be necessary to wear a gauze pad or mini-pad to prevent the drainage from soiling clothes. Bowel movements will not affect healing.
What are the chances of a recurrence of an abscess or fistula?
If properly healed, the problem will usually not return. However, it is important to follow the directions of a colon and rectal surgeon to help prevent recurrence.
Anal Cancer
What is anal cancer?
Cancer describes a set of diseases in which normal cells in the body, through a series of genetic changes, lose the ability to control their growth. As cancers grow, they invade the tissues around them (local invasion). They may also spread to other locations in the body via the blood vessels or lymphatic channels where they may implant and grow (metastases).
The anal canal is a passage that connects the rectum to the outside of the body. The anal canal is surrounded by muscles that keep the anal canal closed except for when the muscles are relaxed during a bowel movement. Anal cancer arises from the cells around the anal opening or in the anal canal just inside the anal opening. Anal cancers arise from skin cells and are called squamous cell carcinomas. Cells that are becoming malignant but have not invaded deep to the skin are referred to as “high-grade dysplasia”, “carcinoma-in-situ” or “Bowen’s disease”.
How common is anal cancer?
Anal cancer is fairly uncommon. It accounts for about 1-2% of gastrointestinal cancers. About 4,000 new cases of anal cancer are diagnosed each year in the U.S.A., about half in women. Approximately 600 people will die of the disease each year. This may be compared to 140,000 new cases of colorectal cancer with 50,000 deaths per year.
Who is at risk?
Anal cancer is commonly associated with the human papillomavirus (HPV). This virus causes warts in and around the anus and on the cervix in women. It is associated with an increased risk of cervical cancer in women.
A risk factor is something that increases a person’s chance of getting a disease. In addition to exposure to the human papillomavirus, additional risk factors include:
- Age – Most people with anal cancer are over 50 years old.
- Anal sex – Persons who participate in anal sex are at an increased risk.
- Smoking – Harmful chemicals from smoking increase the risk of most cancers including anal cancer.
- Immunosuppression – People with weakened immune systems, such as transplant patients who must take drugs to suppress their immune systems and patients with HIV (human immunodeficiency virus) infection, are at a somewhat higher risk.
- Chronic local inflammation – People with long-standing anal fistulas or open wounds are at a slightly higher risk.
- Pelvic radiation – People who have had pelvic radiation therapy for rectal, prostate, bladder or cervical cancer are at an increased risk.
Can anal cancer be prevented?
Few cancers can be totally prevented but your risk may be decreased significantly by reducing your risk factors and by getting regular checkups. Avoid anal sex and infection with HPV and HIV. Use condoms whenever having any kind of intercourse. Although condoms do not eliminate the risk of infection, they do reduce it. Stopping smoking lowers the risk of many types of cancer, including anal cancer.
Anal cancer screening may be performed in high-risk individuals. Anal cancer screening may include an anal Pap smear or anoscopy. An anal pap smear is the same type of test used to screen women for cervical cancer. A swab is passed into the anal canal and cells that come off on the swab are examined under a microscope. Anoscopy is the evaluation of the anal canal using a special scope that allows the physician to visually examine the lining of the anal canal. Any individual with an abnormal anal pap smear should have a follow-up anoscopy to examine the anal canal.
People who are at increased risk should talk to their doctors about anal cancer screening. Individuals who are at particularly increased risk include HIV-positive men, men who have sex with men, individuals with multiple sexual partners and women with a history of cervical warts or precancerous changes identified in the cervix.
What are the symptoms of anal cancer?
Many cases of anal cancer can be found early. Anal cancers form in a part of the digestive tract that the doctor can see and reach easily. Anal cancers often cause symptoms such as:
- Bleeding from the rectum or anus
- The feeling of a lump or mass at the anal opening
- Pain in the anal area
- Persistent or recurrent itching
- Change in bowel habits (having more or fewer bowel movements) or increased straining during a bowel movement
- Narrowing of the stools
- Discharge (mucus or pus) from the anus
- Swollen lymph nodes (glands) in the anal or groin areas.
These symptoms can also be caused by less serious conditions such as hemorrhoids but you should never assume this. If you have any of these symptoms, see your doctor.
How is anal cancer diagnosed?
An abnormal anal pap smear or the presence of symptoms should lead to an examination of the anal canal. If an abnormal area is identified based on your doctor’s exam, a biopsy will be performed to determine the diagnosis. If the diagnosis of cancer is confirmed, additional tests to determine the extent of cancer may be recommended.
How are anal cancers treated?
Treatment for most cases of anal cancer is very effective. There are 3 basic types of treatment used for anal cancer:
- surgery – an operation to remove the cancer
- radiation therapy – high-dose x-rays to kill cancer cells, and
- chemotherapy – giving drugs to kill cancer cells.
Combination therapy including radiation therapy and chemotherapy is now considered the standard treatment for most anal cancers. Occasionally a very small or early tumor may be removed surgically (local excision), with minimal damage to the anal sphincter muscles.
Will I need a colostomy?
The majority of patients treated for anal cancer will not need a colostomy. If the tumor does not respond completely to combination therapy, if it recurs after treatment, or if it is an unusual type, removal of the rectum and anus and creation of a colostomy may be necessary. This operation is known as an abdomino-perineal resection (APR).
What happens after treatment for anal cancer?
Follow-up care to assess the results of treatment and to check for recurrence is very important. Most anal carcinomas are effectively treated. In addition, many tumors that recur may be successfully treated if they are caught early. A careful examination by an experienced physician at regular intervals is the most important method of follow-up. Additional studies may be recommended. You should report any symptoms or problems to your doctor right away.
Conclusion
Anal cancers are unusual tumors arising from the skin or mucosa of the anal canal. As with most cancers, early detection is associated with excellent survival. Most tumors are well treated with combination chemotherapy and radiation. Recurrences may often be treated successfully. Follow the recommended screening examinations for anal and colorectal cancer and consult your doctor early when any anorectal symptoms occur.
Anal Fecal Incontinence
What is incontinence?
Incontinence is the impaired ability to control gas or stool. Its severity ranges from mild difficulty with gas control to severe loss of control over liquid and formed stools. Incontinence to stool is a common problem, but often it is not discussed due to embarrassment.
What causes incontinence?
There are many causes of incontinence. Injury during childbirth is one of the most common causes. These injuries may cause a tear in the anal muscles. The nerves supplying the anal muscles may also be injured. While some injuries may be recognized immediately following childbirth, many others may go unnoticed and will not become a problem until later in life. In these ¬situations, a prior childbirth may not be recognized as the cause of incontinence.
Anal operations or traumatic injury to the tissue surrounding the anal region similarly can damage the anal muscles and hinder bowel control. Some individuals experience loss of strength in the anal muscles as they age. As a result, a minor control problem in a younger person may become more significant later in life.
Diarrhea may be associated with a feeling of urgency or stool leakage due to the frequent ¬liquid stools passing through the anal opening. If bleeding accompanies lack of bowel control, ¬consult your physician. These symptoms may indicate inflammation within the colon (colitis), a rectal tumor, or rectal prolapse – all conditions that require prompt evaluation by a physician.
How is the cause of incontinence determined?
An initial discussion of the problem with your physician will help establish the degree of control difficulty and its impact on your lifestyle. Many clues to the origin of incontinence may be found in patient histories. For example, a woman’s history of past childbirths is very important. Multiple pregnancies, large weight babies, forceps deliveries, or episiotomies may contribute to muscle or nerve injury at the time of childbirth. In some cases, medical illnesses and medications play a role in problems with control.
A physical exam of the anal region should be performed. It may readily identify an obvious injury to the anal muscles. In addition, an ultrasound probe can be used within the anal area to provide a picture of the muscles and show areas in which the anal muscles have been injured.
Frequently, additional studies are required to define the anal area more completely. In a test called anal manometry, a small catheter is placed into the anus to record pressure as patients relax and tighten the anal muscles. This test can demonstrate how weak or strong the muscle really is. A separate test may also be conducted to determine if the nerves that go to the anal muscles are functioning properly.
What can be done to correct the problem?
Treatment of incontinence may include:
- Dietary changes
- Constipating medications
- Muscle strengthening exercises
- Biofeedback
- Surgical muscle repair
- Anal sphincter stimulation
- Sacral nerve stimulation
After a careful history, physical examination and testing to determine the cause and severity of the problem, treatment can be addressed. Mild problems may be treated very simply with dietary changes and the use of some constipating medications. Diseases which cause inflammation in the rectum, such as colitis, may contribute to anal control problems. Treating these diseases also may eliminate or improve symptoms of incontinence. Sometimes a change in prescribed medications may help. Your physician also may recommend simple home exercises that may strengthen the anal muscles to help in mild cases. A type of physical therapy called biofeedback can be used to help patients sense when stool is ready to be evacuated and help strengthen the muscles.
Injuries to the anal muscles may be repaired with surgery. Some individuals may benefit from a technique that delivers electrical energy to the skin and muscles surrounding the anus which results in firming and thickening of this area to help with continence.
In certain individuals that have nerve damage or anal muscles that are damaged beyond repair, an artificial sphincter may be implanted. The artificial sphincter is a plastic, fluid filled doughnut that is surgically implanted around the damaged anal sphincter. This artificial sphincter keeps the anal canal closed. When an individual wants to have a bowel movement, the fluid can be pumped out of the doughnut to allow the anal canal to open.
In extreme cases, patients may find that a colostomy is the best option for improving their quality of life.
Anal Fissure
What is an anal fissure?
An anal fissure is a small tear or cut in the skin that lines the anus. Fissures typically cause pain and often bleed. Fissures are quite common, but are often confused with other causes of pain and bleeding, such as hemorrhoids.
 A simple acute fissure, transanal view.
A simple acute fissure, transanal view.
What are the symptoms of an anal fissure?
The typical symptoms of an anal fissure are pain during or after defecation and bleeding. Patients may try to avoid defecation because of the pain.
What causes an anal fissure?
Trauma: anything that can cut or irritate the inner lining of the anus can cause a fissure. A hard, dry bowel movement is typically responsible for a fissure. Other causes of a fissure include diarrhea or inflammatory conditions of the anal area. Anal fissures may be acute (recent onset) or chronic (present for a long time or recurring frequently). Chronic fissures often have a small external lump associated with the tear called a sentinel pile or skin tag.
How can a fissure be treated?
Often treating one’s constipation or diarrhea can cure a fissure. An acute fissure is typically managed with non-operative treatments and over 90% will heal without surgery. A high fiber diet, bulking agents (fiber supplements), stool softeners, and plenty of fluids help relieve constipation, promote soft bowel movements, and aide in the healing process. Increased dietary fiber may also help to improve diarrhea. Warm baths for 10-20 minutes several times each day are soothing and promote relaxation of the anal muscles, which can also help healing. Occasionally, special medications may be recommended. A chronic fissure may require additional treatment.
Will the problem return?
Fissures can recur easily, and it is quite common for a healed fissure to recur after a hard bowel movement. Even after the pain and bleeding has disappeared one should continue to aim for good bowel habits and adhere to a high fiber diet or fiber supplement regimen. If the problem returns without an obvious cause, further assessment may be needed.
What can be done if a fissure doesn’t heal?
A fissure that fails to respond to treatment should be re-examined. Persistent hard or loose bowel movements, scarring, or spasm of the internal anal sphincter muscle all contribute to delayed healing. Other medical problems such as inflammatory bowel disease, infections, or anal growths (skin tumors) can cause fissure-like symptoms, and patients suffering from persistent anal pain should be examined to exclude these conditions.
What does surgery involve?
Surgery is a highly effective treatment for a fissure and recurrence rates after surgery are low. Surgery usually consists of a small operation to cut a portion of the internal anal sphincter muscle (a lateral internal sphincterotomy). This helps the fissure heal and decreases pain and spasm.
If a sentinel pile is present, it too may be removed to promote healing of the fissure. A sphincterotomy rarely interferes with one’s ability to control bowel movements and is most commonly performed as a short outpatient procedure. Surgical treatments do have other risks, and your surgeon will address these with you.
A chronic fissure with a skin tag and a
hypertrophied anal papilla, coronal view.
How long does the healing process take after surgery?
Complete healing occurs in a few weeks, although pain often disappears after a few days.
Can fissures lead to colon cancer?
No! Persistent symptoms, however, need careful evaluation since conditions other than fissure can cause similar symptoms. Your doctor may request additional testing even if your fissure has successfully healed. A colonoscopy may be required to exclude other causes of bleeding.
Anal Warts
Anal warts (also called “condyloma acuminata”) are a condition that affects the area around and inside the anus. They may also affect the skin of the genital area. They first appear as tiny spots or growths, perhaps as small as the head of a pin, and may grow larger than the size of a pea. Usually, they do not cause pain or discomfort to afflicted individuals. As a result, patients may be unaware that the warts are present. Some patients will experience symptoms such as itching, bleeding, mucus discharge and/or a feeling of a lump or mass in the anal area.
Anal warts, thought to be caused by the human papilloma virus, can grow larger and spread if not removed.
What causes these warts?
They are thought to be caused by the human papilloma virus (HPV) which is transmitted from person to person by direct contact. HPV is considered a sexually transmitted disease. You do not have to have anal intercourse to develop anal condyloma.
Do these warts always need to be removed?
Yes. If they are not removed, the warts usually grow larger and multiply. If left untreated, the warts may lead to an increased risk of cancer in the affected area.
What treatments are available?
If warts are very small and are located only on the skin around the anus, they may be treated with a topical medication. They may also be treated by a physician by freezing the warts with liquid nitrogen. Warts may also be removed surgically. Surgery provides immediate results but must be performed using either a local anesthetic – such as novocaine – or a general or spinal anesthetic, depending on the number and exact location of warts being treated. Warts inside the anal canal usually are not suitable for treatment by medications, and in most cases need to be treated surgically.
Must I be hospitalized for surgical treatment?
No. Surgical treatment of anal warts is usually performed as outpatient surgery.
How much time will I lose from work after surgical treatment?
Most people are moderately uncomfortable for a few days after treatment, and pain medication may be prescribed. Depending on the extent of the disease, some people return to work the next day, while others may remain out of work for several days.
Will a single treatment cure the problem?
Recurrent warts are common. The virus that causes the warts can live concealed in tissues that appear normal for several months before another wart develops. As new warts develop, they usually can be treated in the physician’s office. Sometimes new warts develop so rapidly that office treatment would be quite uncomfortable. In these situations, a second and occasionally third outpatient surgical visit may be recommended.
How long is treatment usually continued?
Follow-up visits are necessary at frequent intervals for several months after the last wart is observed to be certain that no new warts occur.
What can be done to avoid getting these warts again?
In some cases, warts may recur repeatedly after successful removal, since the virus that causes the warts often persists in a dormant state in body tissues. Discuss with you physician how often you should be evaluated for recurrent warts. Abstain from sexual contact with individuals who have anal (or genital) warts. Since many individuals may be unaware that they suffer from this condition, sexual abstinence, condom protection or limiting sexual contact to single partner will reduce your potential exposure to the contagious virus that causes these warts. As a precaution, sexual partners ought to be checked, even if they have no symptoms.
Colonoscopy
What is colonoscopy?
Colonoscopy is a safe, effective method of examining the full lining of the colon and rectum, using a long, flexible, tubular instrument. It is used to diagnose colon and rectum problems and to perform biopsies and remove colon polyps. Most colonoscopies are done on an outpatient basis with minimal inconvenience and discomfort.
Who should have a colonoscopy?
Colonoscopy is routinely recommended to adults 50 years of age or older as part of a colorectal cancer screening program. Patients with a family history of colon or rectal cancer may have their colonoscopy at age 40. Your physician may also recommend a colonoscopy exam if you have change in bowel habit or bleeding, indicating a possible problem in the colon or rectum.
A colonoscopy may be necessary to:
- Check unexplained abdominal symptoms
- Check inflammatory bowel disease (colitis)
- Verify findings of polyps or tumors located with a barium enema exam
- Examine patients who test positive for blood in the stool
- Monitor patients with a personal or family history of colon polyps or cancer.
How is colonoscopy performed?
The bowel must first be thoroughly cleared of all residue before a colonoscopy. This is done one to two days before the exam with a preparation prescribed by your physician.
Many patients receive intravenous sedation, or “twilight sleep” for this procedure. The colonoscope is inserted into the rectum and is advanced to the portion of the colon where the small intestine joins the colon. During a complete examination of the bowel, your physician will remove polyps or take biopsies as necessary.
The entire procedure usually takes less than an hour. Following the colonoscopy, there may be slight discomfort, which quickly improves with the expelling of gas. Most patients can resume their regular diet and activities the same day.
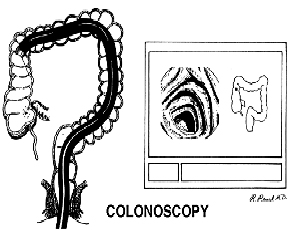
Left: Flexible fiberoptic colonoscope in place examining the lining of the colon.
Right: Image of the portion of the colon being examined on the television monitor.
What are the benefits of colonoscopy?
Colonoscopy is more accurate than an x-ray exam of the colon to detect polyps or early cancer. With colonoscopy, it is now possible to detect and remove most polyps without abdominal surgery. Removing polyps is an important step in the prevention of colon cancer.
What are the risks of colonoscopy?
Colonoscopy is a very safe procedure with complications occurring in less than 1% of patients. These risks include bleeding, a tear in the intestine, risks of anesthesia and failure to detect a polyp.
Colon Rectal Surgery
Bowel Resection
Done open (with a larger cut in the abdomen) or laparoscopically (laparoscopic bowel resection is performed with the aid of a small camera and instruments placed through straw-like tubes passed into the abdomen), bowel resection is a procedure during which a diseased part of the large intestine (colon) or rectum is removed.
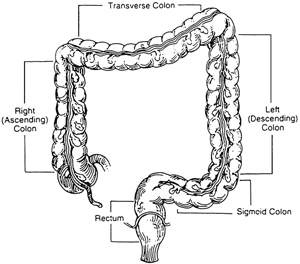
Diverticulosis and Diverticulitis
Removal of part of the colon may be needed when a portion of the colon, usually the sigmoid colon, suffers from infection from diverticular disease. Diverticula are outpouchings of the bowel which are present in more than half of American adults. When infected, these pouches can cause pain and fever. At times, a rupture of the colon can occur.
Colon and Rectal Cancer
Removal of colon or rectum may be needed to remove cancer and enable cure and relief of symptoms. Again, the procedure is often done laparoscopically (see above).
Crohn’s Disease
Medical management and surgical management can be provided as indicated by the disease symptoms. St. Luke’s Colon and Rectal Surgeons work in conjunction with our Gastroenterological colleagues in maximizing medical management in cases where surgery can be avoided or delayed safely.
Ulcerative Colitis surgery–Ileal Pouch-anal Anastomosis–IPAA
A proctocolectomy is a procedure to remove all of the colon and rectum for patients with ulcerative colitis. The surgeon forms a pouch from the end of the small intestine (the ileum) and attaches it to the anus to maintain the digestive tract continuity. This ileal pouch becomes the digestive tract’s waste reservoir, which functions similar to the rectum. Laparoscopic surgical techniques can be applied to this operation.
Hemorrhoidectomy and alternatives
Options to surgical removal of the hemorrhoids include rubber banding in the office when the hemorrhoids are smaller, and circular stapling of the hemorrhoids internally when the outside hemorrhoids are relatively normal. The procedure for prolapse and hemorrhoids (PPH) uses a stapler to reposition the anal canal tissue and reduces blood flow to the hemorrhoids, causing them to shrink. It should be noted that we can often avoid surgery with dietary management.
Trans-Anal Endoscopic Microsurgery
A procedure to remove rectal lesions using endoscopes, which are small, lighted instruments that contain cameras. This can often access small tumors through the anus to avoid large and disfiguring abdominal operations.
Anal Sphincter Repair
This procedure can return function of the anus to restore continence (control) of the feces. Commonly, this operation is offered for leakage of stool related to earlier injury of the anus at childbirth.
Rectal prolapse surgery is also offered for conditions, most often in women, where pelvic floor and rectal prolapse lead to constipation, discomfort, and pain.
**With a diverse group of Colon and Rectal training backgrounds from Mayo Clinic, The University of Illinois at Chicago, Hahnemann University Hospital, and Lehigh Valley Hospital Colorectal Residencies, our surgeons bring state-of-the-art care to our patients.
Colorectal Cancer
Colorectal cancer is the second most common cancer in the United States, striking 140,000 people annually and causing 60,000 deaths. That’s a staggering figure when you consider the disease is potentially curable if diagnosed in the early stages.
Who is at risk?
Though colorectal cancer may occur at any age, more than 90% of the patients are over age 40, at which point the risk doubles every ten years. In addition to age, other high-risk factors include a family history of colorectal cancer and polyps and a personal history of ulcerative colitis, colon polyps or cancer of other organs, especially of the breast or uterus.
How does it start?
It is generally agreed that nearly all colon and rectal cancer begins in benign polyps. These pre-malignant growths occur on the bowel wall and may eventually increase in size and become cancer. Removal of benign polyps is one aspect of preventive medicine that really works!
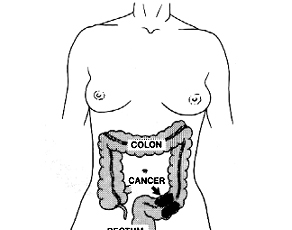 What are the symptoms?
What are the symptoms?
The most common symptoms are rectal bleeding and changes in bowel habits, such as constipation or diarrhea. (These symptoms are also common in other diseases so it is important you receive a thorough examination should you experience them.) Abdominal pain and weight loss are usually late symptoms indicating possible extensive disease.
Unfortunately, many polyps and early cancers fail to produce symptoms. Therefore, it is important that your routine physical includes colorectal cancer detection procedures once you reach age 50. There are several methods for the detection of colorectal cancer. These include a digital rectal examination, a chemical test of the stool for blood, flexible sigmoidoscopy and colonoscopy (lighted tubular instruments used to inspect the lower bowel) and barium enema. Be sure to discuss these options with your surgeon to determine which procedure is best for you. Individuals who have a first-degree relative (parent or sibling) with colon cancer or polyps should start their colon cancer screening at the age of 40.
How is colorectal cancer treated?
Colorectal cancer requires surgery in nearly all cases for complete cure. Radiation and chemotherapy are sometimes used in addition to surgery. Between 80-90% are restored to normal health if the cancer is detected and treated in the earliest stages. The cure rate drops to 50% or less when diagnosed in the later stages. Thanks to modern technology, less than 5% of all colorectal cancer patients require a colostomy, the surgical construction of an artificial excretory opening from the colon.
Can colon cancer be prevented?
Colon cancer is preventable. The most important step towards preventing colon cancer is getting a screening test. Any abnormal screening test should be followed by a colonoscopy. Some individuals prefer to start with colonoscopy as a screening test.
Colonoscopy provides a detailed examination of the bowel. Polyps can be identified and can often be removed during colonoscopy.
Though not definitely proven, there is some evidence that diet may play a significant role in preventing colorectal cancer. As far as we know, a high fiber, low-fat diet is the only dietary measure that might help prevent colorectal cancer.
Finally, pay attention to changes in your bowel habits. Any new changes such as persistent constipation, diarrhea, or blood in the stool should be discussed with your physician.
Can hemorrhoids lead to colon cancer?
No, but hemorrhoids may produce symptoms similar to colon polyps or cancer. Should you experience these symptoms, you should have them examined and evaluated by a physician, preferably by a colon and rectal surgeon.
Colorectal Cancer Surgery-Follow Up Evaluation
Why should there be a postoperative follow-up program?
Surgery is the most effective treatment for colorectal cancer. Even when all visible cancer has been removed, it is possible for cancer cells to be present in other areas of the body. These cancer deposits, when very small, are undetectable at the time of surgery, but they can begin to grow at a later time. The chance of recurrence depends on the characteristics of the original cancer and the effectiveness of chemotherapy, if needed, or other follow up treatment. Patients with recurrent cancers – if diagnosed early – may benefit, or be cured, by further surgery or other treatment.
Another good reason for postoperative follow up is to look for new colon or rectal polyps. Approximately one in five patients who has had colon cancer will develop a new polyp at a later time in life. It is important to detect and remove these polyps before they become cancerous.
How long will my follow-up program last?
Most recurrent cancers are detected within the first two years after surgery. Therefore, follow up is most frequent during this period of time. After five years, nearly all cancers that are going to recur will have done so. Follow up after five years is primarily to detect new polyps, and can, therefore, be less frequent but advisable for life.
What might I expect at my follow-up visit?
Your doctor will examine you approximately every two or three months for the first two years, and discuss your progress. A CEA blood test can be done, as a method of trying to detect recurrence of cancer. Because this test is not totally reliable, other follow up examinations may be advised. These examinations may include flexible sigmoidoscopy (an examination of the rectum and lower colon with a flexible, lighted instrument), colonoscopy (examination of the entire colon with a long flexible instrument), chest x-rays, and sometimes CT scans or ultrasound tests.
What about my family?
Close relatives of patients with colon and rectal cancer (parents, brothers, sisters, children) are at increased risk for the disease. Because of this, periodic examination of the lining of the colon, using a colonoscope to detect small polyps, is advised. If polyps are promptly detected and removed, cancers cannot develop. Other factors which increase the risk of developing polyps or cancer include cancer occurring at an early age, and a personal history of breast or female genital cancer.
Constipation
What is constipation?
Constipation word cloud concept
Constipation is a symptom that has different meanings to different individuals. Most commonly, it refers to infrequent bowel movements, but it may also refer to a decrease in the volume or weight of stool, the need to strain to have a movement, a sense of incomplete evacuation, or the need for enemas, suppositories or laxatives in order to maintain regularity.
For most people, it is normal for bowel movements to occur from three times a day to three times a week; other people may go a week or more without experiencing discomfort or harmful effects. Normal bowel habits are affected by diet. The average American diet includes 12 to 15 grams of fiber per day, although 25 to 30 grams of fiber and about 60 to 80 ounces of fluid daily are recommended for proper bowel function. Exercise is also beneficial to proper function of the colon.
About 80 percent of people suffer from constipation at some time during their lives, and brief periods of constipation are normal. Constipation may be diagnosed if bowel movements occur fewer than three times weekly on an ongoing basis. Widespread beliefs, such as the assumption that everyone should have a movement at least once each day, have led to overuse and abuse of laxatives.
Eating foods high in fiber, including bran, shredded wheat, whole grain breads and certain fruits and vegetables will help provide the 25 to 30 grams of fiber per day recommended for proper bowel function.
What causes constipation?
There may be several, possibly simultaneous, causes for constipation, including inadequate fiber and fluid intake, a sedentary lifestyle, and environmental changes. Constipation may be aggravated by travel, pregnancy or change in diet. In some people, it may result from repeatedly ignoring the urge to have a bowel movement.
More serious causes of constipation include growths or areas of narrowing in the colon, so it is wise to seek the advice of a colon and rectal surgeon when constipation persists. Individuals with spinal cord injuries frequently experience problems with constipation. Constipation may be a symptom of diabetes. Constipation may also be associated with scleroderma, or disorders of the nervous or endocrine systems, including thyroid disease, multiple sclerosis, or Parkinson’s disease.
Can medication cause constipation?
Yes, many medications, including pain killers, antidepressants, tranquilizers, and other psychiatric medications, blood pressure medication, diuretics, iron supplements, calcium supplements, and aluminum containing antacids can slow the movement of the colon and worsen constipation.
When should I see a doctor about constipation?
Any persistent change in bowel habit, increase or decrease in frequency or size of stool or increased difficulty in evacuating warrants evaluation. Whenever constipation symptoms persist for more than three weeks, you should consult your physician. If blood appears in the stool, consult your physician right away.
How can the cause of constipation be determined?
Constipation may have many causes, and it is important to identify them so that treatment can be as simple and specific as possible. Your doctor will want to check for any anatomic causes, such as growths or areas of narrowing in the colon.
Digital examination of the anorectal area is usually the first step, since it is relatively simple and may provide clues to the underlying causes of the problem. Examination of the intestine with either a flexible lighted instrument or barium x-ray study may help pinpoint the problem and exclude serious conditions known to cause constipation, such as polyps, tumors, or diverticular disease. If an anatomic problem is identified, treatment can be directed toward correcting the abnormality.
Other tests may identify specific functional causes to help direct treatment. For example, “marker studies,” in which the patient swallows a capsule containing markers that show up on x-rays taken repeatedly over several days, may provide clues to disorders in muscle function within the intestine. Other physiologic tests evaluate the function of the anus and rectum. These tests may involve evaluating the reflexes of anal muscles that control bowel movements using a small plastic catheter, or x-ray testing to evaluate function of the anus and rectum during defecation.
In many cases, no specific anatomic or functional causes are identified and the cause of constipation is said to be nonspecific.
How is constipation treated?
The vast majority of patients with constipation are successfully treated by adding high fiber foods like bran, shredded wheat, whole grain breads and certain fruits and vegetables to the diet, along with increased fluids. Your physician may also recommend lifestyle changes. Fiber supplements containing indigestible vegetable fiber, such as bran, are often recommended and may provide many benefits in addition to relief of constipation. They may help to lower cholesterol levels, reduce the risk of developing colon polyps and cancer, and help prevent symptomatic hemorrhoids.
Fiber supplements may take several weeks, possibly months, to reach full effectiveness, but they are neither harmful nor habit forming, as some stimulant laxatives may become with overuse or abuse. Other types of laxatives, enemas or suppositories should be used only when recommended and monitored by your colon and rectal surgeon.
Designating a specific time each day to have a bowel movement also may be very helpful to some patients. In some cases, bio-feedback may help to retrain poorly functioning anal sphincter muscles. Only in rare circumstances are surgical procedures necessary to treat constipation. Your colon and rectal surgeon can discuss these options with you in greater detail to determine the best treatment for you.
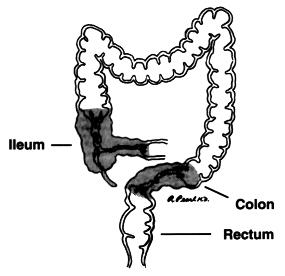
Crohn’s Disease
Crohn’s disease is a chronic inflammatory process primarily involving the intestinal tract. Although it may involve any part of the digestive tract from the mouth to the anus, it most commonly affects the last part of the small intestine (ileum) and/or the large intestine (colon and rectum).
Crohn’s disease is a chronic condition and may recur at various times over a lifetime. Some people have long periods of remission, sometimes for years, when they are free of symptoms. There is no way to predict when a remission may occur or when symptoms will return.
 What are the symptoms of Crohn’s disease?
What are the symptoms of Crohn’s disease?
Because Crohn’s disease can affect any part of the intestine, symptoms may vary greatly from patient to patient. Common symptoms include cramping, abdominal pain, diarrhea, fever, weight loss, and bloating. Not all patients experience all of these symptoms, and some may experience none of them. Other symptoms may include anal pain or drainage, skin lesions, rectal abscess, fissure, and joint pain (arthritis).
Common Crohn’s symptoms:
- Cramping – abdominal pain
- Diarrhea
- Fever
- Weight loss
- Bloating
- Anal pain or drainage
- Skin lesions
- Rectal abscess
- Fissure
- Joint pain
Who does it affect?
Any age group may be affected, but the majority of patients are young adults between 16 and 40 years old. Crohn’s disease occurs most commonly in people living in northern climates. It affects men and women equally and appears to be common in some families. About 20 percent of people with Crohn’s disease have a relative, most often a brother or sister, and sometimes a parent or child, with some form of inflammatory bowel disease.
Crohn’s disease and a similar condition called ulcerative colitis are often grouped together as inflammatory bowel disease. The two diseases afflict an estimated two million individuals in the U.S.
What causes Crohn’s disease?
The exact cause is not known. However, current theories center on an immunologic (the body’s defense system) and/or bacterial cause. Crohn’s disease is not contagious, but it does have a slight genetic (inherited) tendency. An x-ray study of the small intestine may be used to diagnose Crohn’s disease.
How is Crohn’s disease treated?
Initial treatment is almost always with medication. There is no “cure” for Crohn’s disease, but medical therapy with one or more drugs provides a means to treat early Crohn’s disease and relieve its symptoms. The most common drugs prescribed are corticosteroids, such as prednisone and methylprednisolone, and various anti-inflammatory agents.
Other drugs occasionally used include 6-mercaptopurine and azathioprine, which are immunosuppressive. Metronidazole, an antibiotic with immune system effects, is frequently helpful in patients with anal disease.
In more advanced or complicated cases of Crohn’s disease, surgery may be recommended. Emergency surgery is sometimes necessary when complications, such as a perforation of the intestine, obstruction (blockage) of the bowel, or significant bleeding occur with Crohn’s disease. Other less urgent indications for surgery may include abscess formation, fistulas (abnormal communications from the intestine), severe anal disease or persistence of the disease despite appropriate drug treatment.
Not all patients with these or other complications require surgery. This decision is best reached through consultation with your gastroenterologist and your colon and rectal surgeon.
Shouldn’t surgery for Crohn’s disease be avoided at all costs?
While it is true that medical treatment is preferred as the initial form of therapy, it is important to realize that surgery is eventually required in up to three-fourths of all patients with Crohn’s. Many patients have suffered unnecessarily due to a mistaken belief that surgery for Crohn’s disease is dangerous or that it inevitably leads to complications.
Surgery is not “curative,” although many patients never require additional operations. A conservative approach is frequently taken, with a limited resection of intestine (removal of the diseased portion of the bowel) being the most common procedure.
Surgery often provides effective long-term relief of symptoms and frequently limits or eliminates the need for ongoing use of prescribed medications. Surgical therapy is best conducted by a physician skilled and experienced in the management of Crohn’s disease.
Diverticular Disease
Diverticulosis of the colon is a common condition that afflicts about 50 percent of Americans by age 60 and nearly all by age 80. Only a small percentage of those with diverticulosis have symptoms, and even fewer will ever require surgery.
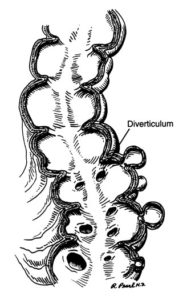
What is Diverticulosis/ Diverticulitis?
Diverticula are pockets that develop in the colon wall, usually in the sigmoid or left
colon, but may involve the entire colon. Diverticulosis describes the presence of these pockets. Diverticulitis describes inflammation or complications of these pockets.
What are the symptoms of diverticular disease?
Uncomplicated diverticular disease is usually not associated with symptoms. Symptoms are related to complications of diverticular disease including diverticulitis and bleeding. Diverticular disease is a common cause of significant bleeding from the colon.
Diverticulitis – an infection of the diverticula – may cause one or more of the following symptoms: pain in the abdomen, chills, fever and change in bowel habits. More intense symptoms are associated with serious complications such as perforation (rupture), abscess or fistula formation (an abnormal connection between the colon and another organ or the skin).
What is the cause of diverticular disease?
The cause of diverticulosis and diverticulitis is not precisely known, but it is more common for people with a low fiber diet. It is thought that a low-fiber diet over the years creates increased colon pressure and results in pockets or diverticula.
How is diverticular disease treated?
Increasing the amount of dietary fiber (grains, legumes, vegetables, etc.) – and sometimes restricting certain foods reduces the pressure in the colon and may decrease the risk of complications due to diverticular disease.
Diverticulitis requires different management. Mild cases may be managed with oral antibiotics, dietary restrictions and possibly stool softeners. More severe cases require hospitalization with intravenous antibiotics and dietary restraints. Most acute attacks can be relieved with such methods.
When is surgery necessary?
Surgery is reserved for patients with recurrent episodes of diverticulitis, complications or severe attacks when there’s little or no response to medication. Surgery may also be required in individuals with a single episode of severe bleeding from diverticulosis or with recurrent episodes of bleeding.
Surgical treatment for diverticulitis removes the diseased part of the colon, most commonly, the left or sigmoid colon. Often the colon is hooked up or “anastomosed” again to the rectum. Complete recovery can be expected. Normal bowel function usually resumes in about three weeks. In emergency surgeries, patients may require a temporary colostomy bag. Patients are encouraged to seek medical attention for abdominal symptoms early to help avoid complications.
Genetics And Colorectal Cancer
What does genetics have to do with colon and rectal cancer?
Genes are the biochemical information that we inherit from each of our parents. They determine our varied physical features and may predispose us to certain diseases. Probably all cancers, especially colon and rectal cancer (CRC), have hereditary genetic factors that potentially increase an individual’s risk to developing these malignancies. In other words, genes are the reason why some diseases such as CRC occur more frequently in certain families. For this reason, when visiting a colon and rectal surgeon, it is important to provide a detailed family history with regard to cancer.
Are there different types of colon and rectal cancer?
From a genetic perspective, there are three broad classifications of CRC. The table below shows the respective proportion of each different classification.
| Sporadic Colon Cancer | 50-60 % |
| Familial Colon Cancer | 30-40 % |
| Inherited Colon Cancer Syndromes | 4-6 % |
What is sporadic colon cancer?
Sporadic colon cancer generally occurs in someone over age 60, without a prior family history of CRC. One in eighteen Americans will develop CRC. Patients who develop CRC as the first member of their family should be encouraged to inform relatives. People with a family history of colon rectal cancer should be advised to inquire about screening protocols at an earlier age.
What is familial colon cancer?
Some families are predisposed to getting colon cancer. There should be concern if a family has more than one relative with CRC, especially if the CRC occurred in an individual before age 50. If a first degree relative (parent, sibling, or child) develops a colorectal cancer, the risk of family members developing this disease is doubled. Individuals with a first degree relative who has been diagnosed with CRC should begin colon cancer screening at 40 years of age or 10 years earlier than the age at which their relative was diagnosed with cancer, whichever is earlier.
What are hereditary colorectal cancers?
Hereditary colorectal cancers are associated with a specific genetic abnormality. As genetic researchers continue to define certain syndromes, more genes that predispose colorectal cancer will likely be identified. Currently, some of the syndromes include:
- HNPCC (Hereditary Non-Polyposis Colon Cancer, Lynch Syndrome)
- FAP (Familial Adenomatous Polyposis)
- aFAP (Attenuated Familial Adenomatous Polyposis)
- APCI 1307K
- Peutz-Jehger’s Syndrome
- MAP (MYH associated Polyposis)
- Juvenile Polyposis
- Hereditary Polyposis
What type of information regarding family history should I tell my colon and rectal surgeon?
Family history information regarding the following items will allow your colon and rectal surgeon to formulate the best plan for prevention and treatment.
- All family members and their approximate ages of when they were diagnosed with colorectal polyps or cancer
- Family history of gynecologic cancers (ovarian or uterine)
What will the colon and rectal surgeon do with this information?
The colon and rectal surgeon will use this information to assess an individual’s risk for CRC. Additional evaluation of an individual may help to detect and identify a family cancer syndrome. Recommendations for this analysis may include colonoscopy, genetic counseling, formal generic testing, regular follow-up examination, and potential referral to other medical specialists.
Hemorrhoids
Did you know…
- Hemorrhoids are one of the most common ailments known.
- More than half the population will develop hemorrhoids, usually after age 30.
- Millions of Americans currently suffer from hemorrhoids.
- The average person suffers in silence for a long period before seeking medical care.
- Today’s treatment methods make some types of hemorrhoid removal much less painful.
What are hemorrhoids?
Often described as “varicose veins of the anus and rectum”, hemorrhoids are enlarged, bulging blood vessels in and about the anus and lower rectum. There are two types of hemorrhoids: external and internal, which refer to their location.
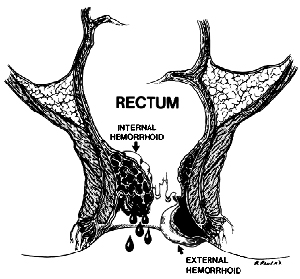 External (outside) hemorrhoids develop near the anus and are covered by very sensitive skin. These are usually painless. However, if a blood clot (thrombosis) develops in an external hemorrhoid, it becomes a painful, hard lump. The external hemorrhoid may bleed if it ruptures.
External (outside) hemorrhoids develop near the anus and are covered by very sensitive skin. These are usually painless. However, if a blood clot (thrombosis) develops in an external hemorrhoid, it becomes a painful, hard lump. The external hemorrhoid may bleed if it ruptures.
Internal (inside) hemorrhoids develop within the anus beneath the lining. Painless bleeding and protrusion during bowel movements are the most common symptom. However, an internal hemorrhoid can cause severe pain if it is completely “prolapsed” – protrudes from the anal opening and cannot be pushed back inside.
What causes hemorrhoids?
An exact cause is unknown; however, the upright posture of humans alone forces a great deal of pressure on the rectal veins, which sometimes causes them to bulge. Other contributing factors include:
• Aging
• Chronic constipation or diarrhea
• Pregnancy
• Heredity
• Straining during bowel movements
• Faulty bowel function due to overuse of laxatives or enemas
• Spending long periods of time (e.g., reading) on the toilet
Whatever the cause, the tissues supporting the vessels stretch. As a result, the vessels dilate; their walls become thin and bleed. If the stretching and pressure continue, the weakened vessels protrude.
What are the symptoms?
If you notice any of the following, you could have hemorrhoids:
• Bleeding during bowel movements
• Protrusion during bowel movements
• Itching in the anal area
• Pain
• Sensitive lump(s)
How are hemorrhoids treated?
Mild symptoms can be relieved frequently by increasing the amount of fiber (e.g., fruits, vegetables, breads and cereals) and fluids in the diet. Eliminating excessive straining reduces the pressure on hemorrhoids and helps prevent them from protruding. A sitz bath – sitting in plain warm water for about 10 minutes – can also provide some relief .
With these measures, the pain and swelling of most symptomatic hemorrhoids will decrease in two to seven days, and the firm lump should recede within four to six weeks. In cases of severe or persistent pain from a thrombosed hemorrhoid, your physician may elect to remove the hemorrhoid containing the clot with a small incision. Performed under local anesthesia as an outpatient, this procedure generally provides relief.
Severe hemorrhoids may require special treatment, much of which can be performed on an outpatient basis.
- Ligation – the rubber band treatment – works effectively on internal hemorrhoids that protrude with bowel movements. A small rubber band is placed over the hemorrhoid, cutting off its blood supply. The hemorrhoid and the band fall off in a few days and the wound usually heals in a week or two. This procedure sometimes produces mild discomfort and bleeding and may need to be repeated for a full effect.
- Injection and Coagulation can also be used on bleeding hemorrhoids that do not protrude. Both methods are relatively painless and cause the hemorrhoid to shrivel up.
- Hemorrhoid stapling – this is a technique that uses a special device to internally staple and excise internal hemorrhoidal tissue. The stapling method may lead to shrinkage of but does not remove external hemorrhoids. This procedure is generally more painful that rubber band ligation and less painful than hemorroidectomy.
- Hemorrhoidectomy – surgery to remove the hemorrhoids – is the most complete method for removal of internal and external hemorrhoids. It is necessary when (1) clots repeatedly form in external hemorrhoids; (2) ligation fails to treat internal hemorrhoids; (3) the protruding hemorrhoid cannot be reduced; or (4) there is persistent bleeding. A hemorrhoidectomy removes excessive tissue that causes the bleeding and protrusion. It is done under anesthesia using either sutures or staplers, and may, depending upon circumstances, require hospitalization and a period of inactivity. Laser hemorrhoidectomies do not offer any advantage over standard operative techniques. They are also quite expensive, and contrary to popular belief, are no less painful.
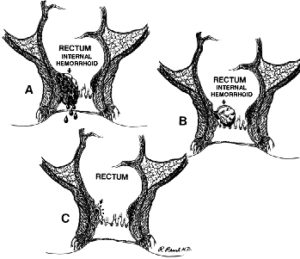
Rubber Band Ligation of Internal Hemorrhoids:
A. Bulging, bleeding, internal hemorrhoid
B. Rubber band applied at the base of the hemorrhoid
C. About 7 days later, the banded hemorrhoid has fallen off leaving a small scar at its base (arrow)
Do hemorrhoids lead to cancer?
No. There is no relationship between hemorrhoids and cancer. However, the symptoms of hemorrhoids, particularly bleeding, are similar to those of colorectal cancer and other diseases of the digestive system. Therefore, it is important that all symptoms are investigated by a physician specially trained in treating diseases of the colon and rectum and that everyone 50 years or older undergo screening tests for colorectal cancer. Do not rely on over-the-counter medications or other self-treatments. See a colorectal surgeon first so your symptoms can be properly evaluated and effective treatment prescribed.
Irritable Bowel Syndrome
WHAT IS IRRITABLE BOWEL SYNDROME?
Irritable bowel syndrome (IBS) is a common disorder that may affect over 15 percent of the general population. It is sometimes referred to as spastic colon, spastic colitis, mucous colitis or nervous stomach. IBS should not be confused with other diseases of the bowel such as ulcerative colitis or Crohn’s disease. IBS is a functional disorder where the function of the bowels may be abnormal but no structural abnormalities exist.
WHAT ARE THE SYMPTOMS OF IBS?
People with IBS may experience abdominal pain and changes in bowel habits – either diarrhea, constipation, or both at different times. Symptoms associated with IBS include abdominal cramps, fullness or bloating, abnormal stool consistency, passage of mucous, urgency or a feeling of incomplete bowel movements.
WHAT CAUSES IBS?
The symptoms of IBS seem to occur as a result of abnormal functioning or communication between the nervous system and the muscles of the bowel. This abnormal regulation may cause the bowel to be “irritated” or more sensitive. The muscles in the bowel wall may contract too forcefully or too weakly, too slowly or rapidly at certain times. Although there is no physical obstruction, a patient may perceive cramps or functional blockage.
Although there is no physical obstruction, a patient
may perceive cramps or functional blockage.
WHAT ROLE DOES STRESS PLAY IN IBS?
IBS is not caused by stress. It is not a psychological or psychiatric disorder, however emotional stress may contribute to IBS. Many people may experience nausea or diarrhea when nervous or anxious. While we may not be able to control the effect stress has on our intestines, reducing the sources of stress in our lives may help to alleviate the symptoms of IBS.
HOW CAN I TELL IF THE PROBLEM IS IBS OR SOMETHING ELSE?
A careful medical history and physical examination by a colon and rectal surgeon or other physician are essential to exclude more serious disorders. Tests may include blood tests, stool tests, visual inspection of the inside of the colon with flexible sigmoidoscopy or colonoscopy, and x-ray studies. Fever, anemia, rectal bleeding and unexplained weight loss are not symptoms of IBS and need to be evaluated by your physician.
HOW IS IBS TREATED?
Understanding that IBS is not a serious or life-threatening condition may relieve anxiety and stress, which often contribute to the problem. Stress reduction, use of behavioral therapy, biofeedback, relaxation or pain management techniques can help relieve the symptoms of IBS in some individuals. Use of a diary may help to identify certain foods or other factors that cause symptoms.
Mild to moderate symptoms can often be managed by dietary changes. Your physician may recommend avoiding meals that are too large or high in fatty or fried foods. Caffeine or alcohol may also cause cramps or diarrhea. Some types of sugar, such as sorbitol commonly used as a low calorie sweetener and fructose, found naturally in honey and some fruits may be poorly absorbed by the gut and cause cramping and diarrhea. Gas producing foods such as beans, cabbage, cauliflower, broccoli, brussel sprouts and onions may cause bloating and increased discomfort in people with IBS.
Increasing dietary fiber may help to improve IBS symptoms. Soluble fiber such as that found in citrus fruits, flaxseeds and legumes may help soften stool and lessen the severity of cramps. Insoluble fiber such as cellulose, cereals and bran can absorb water as it moves through the digestive tract and lessen diarrhea. In some people too much fiber can cause discomfort. Adding fiber to the diet gradually with adequate amounts of liquids may eliminate the discomfort.
Individuals with moderate to severe IBS may benefit from prescribed medication. Medications can help to control the symptoms of IBS but they do not cure the condition. Medications act directly on the intestinal muscles to help the contractions return to normal. Antidepressants in low doses have been shown to be helpful in some with IBS.
HOW LONG DOES THE TREATMENT TAKE TO RELIEVE SYMPTOMS?
Relief of IBS Symptoms is often a slow process. It may take six months or more for definite improvement to be appreciated. Patience is extremely important in dealing with this problem.
The tendency for the intestine to respond to stress will always be present. With attention to proper diet and in some cases, use of appropriate medications, the symptoms of IBS can be greatly improved or eliminated.
CAN IBS LEAD TO MORE SERIOUS PROBLEMS?
IBS does not cause cancer, bleeding or inflammatory bowel diseases, such as ulcerative colitis.
Ostomy
WHAT IS AN OSTOMY?
An ostomy is a surgically created opening connecting an internal organ to the surface of the body. Different kinds of ostomies are named for the organ involved. The most common types of ostomies in intestinal surgery are an “ileostomy” (connecting the ileal part of the small intestine to the abdominal wall) and a “colostomy” (connecting the colon, or, large intestine to the abdominal wall).
An ostomy may be temporary or permanent. A temporary ostomy may be required if the intestinal tract can’t be properly prepared for surgery because of blockage by disease or scar tissue. A temporary ostomy may also be created to allow inflammation or an operative site to heal without contamination by stool. Temporary ostomies can usually be reversed with minimal or no loss of intestinal function. A permanent ostomy may be required when disease, or its treatment, impairs normal intestinal function, or when the muscles that control elimination do not work properly or require removal. The most common causes of these conditions are low rectal cancer and inflammatory bowel disease.
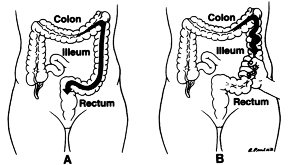
An ostomy connects either the small or the large intestine to the surface of the body.
HOW WILL I CONTROL MY BOWEL MOVEMENTS?
Once your ostomy has been created, your surgeon or wound ostomy continence nurse (a WOC nurse specializes in ostomy care) will teach you to attach and care for a pouch called an ostomy appliance. An ostomy appliance, or pouch, is designed to catch eliminated fecal material (stool). The pouch is made of plastic and is held to the body with an adhesive. The adhesive, in turn, protects the skin from moisture. The pouch is disposable and is emptied or changed as needed. The system is quite secure; “accidents” are not common, and the pouches are odor-free.
Your bowel movements will naturally empty into the pouch. The frequency and quantity of your bowel movements will vary, depending on the type of ostomy you have, your diet, and your bowel habits prior to surgery. You may be instructed to modify your eating habits in order to control the frequency and consistency of your bowel movements. If the ostomy is a colostomy, irrigation techniques may be learned which allow for increased control over the timing of bowel movements.

An ostomy appliance is a plastic pouch, held to the body with an adhesive skin barrier, that provides secure and odor-free control of bowel movements.
WILL OTHER PEOPLE KNOW THAT I HAVE AN OSTOMY?
Not unless you tell them. An ostomy is easily hidden by your usual clothing. You probably have met people with an ostomy and not realized it!
WHERE WILL THE OSTOMY BE?
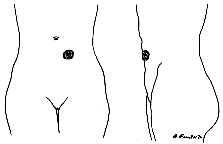
An ostomy is best placed on a flat portion of the abdominal wall. Before undergoing surgery to create an ostomy, it is best for your surgeon or WOC nurse to mark an appropriate place on your abdominal wall not constricted by your belt-line. A colostomy is usually placed to the left of your navel and an ileostomy to the right.
WILL MY PHYSICAL ACTIVITIES BE LIMITED?
The answer to this question is usually no. Public figures, prominent entertainers, and even professional athletes have ostomies that do not significantly limit their activities. All your usual activities, including active sports, may be resumed once healing from surgery is complete.
WILL AN OSTOMY AFFECT MY SEX LIFE?
Most patients with ostomies resume their usual sexual activity. Many people with ostomies worry about how their sexual partner will think of them because of their appliance. This perceived change in one’s body image can be overcome by a strong relationship, time and patience. Support groups are also available in many cities.
WHAT ARE THE COMPLICATIONS OF AN OSTOMY?
Complications from an ostomy can occur. Most, like local skin irritation are typically minor and can be easily remedied. Problems such as a hernia associated with the ostomy or prolapse of the ostomy (a protrusion of the bowel) occasionally require surgery if they cause significant symptoms. Weight loss or gain may affect the function of an ostomy.
Living with an ostomy will require some adjustments and learning, but an active and fulfilling life is still possible and likely. Your colon and rectal surgeon and WOC nurse will provide you with skills and support to help you better live with your ostomy.
WOULD YOU LIKE ADDITIONAL INFORMATION?
More information about ostomies can be found at: www.uoaa.org – The United Ostomy Associations of America
Pelvic Floor Dysfunction
What is pelvic floor dysfunction?
For most people, having a bowel movement is a seemingly automatic function. For some individuals, the process of evacuating stool may be difficult. Symptoms of pelvic floor dysfunction include constipation and the sensation of incomplete emptying of the rectum when having a bowel movement. Incomplete emptying may result in the individual feeling the need to attempt a bowel movement several times within a short period of time. Residual stool left in the rectum may slowly seep out of the rectum leading to reports of bowel incontinence.
The process of defecation (having a bowel movement) requires the coordinated effort of different muscles. The pelvic floor is made up of several muscles that support the rectum like a hammock. When an individual wants to have a bowel movement the pelvic floor muscles are supposed to relax allowing the rectum to empty. While the pelvic floor muscles are relaxing, muscles of the abdomen contract to help push the stool out of the rectum. Individuals with pelvic floor dysfunction have a tendency to contract instead of relax the pelvic floor muscles. When this happens during an attempted bowel movement, these individuals are effectively pushing against an unyielding muscular wall.
How is pelvic floor dysfunction diagnosed?
The diagnosis of pelvic floor disorder starts with a careful history regarding an individual’s symptoms, medical problems and a history of physical or emotional trauma that may be contributing to their problem. Next the physician examines the patient to identify any physical abnormality. A defecating proctogram is a study commonly used to demonstrate the functional problem in a person with pelvic floor dysfunction. During this study, the patient is given an enema of a thick liquid that can be detected with x-ray. A special x-ray video records the movement of the pelvic floor muscles and the rectum while the individual attempts to empty the liquid from the rectum. Normally the pelvic floor relaxes allowing the rectum to straighten and the liquid to pass out of the rectum. This study will demonstrate if the pelvic floor muscles are not relaxing appropriately and preventing passage of the liquid.
The defecating proctogram is also useful to show if the rectum is folding in on itself (rectal prolapse). Many women have outpouching of the rectum known as a rectocele. Usually a rectocele does not affect the passage of stool. In some instances, however, stool may become trapped in a rectocele causing symptoms of incomplete evacuation. The defecating proctogram helps to identify if liquid is getting trapped in a rectocele when the individual is trying to empty the rectum.
How is pelvic floor dysfunction treated?
Pelvic floor dysfunction due to non-relaxation of the pelvic floor muscles may be treated with specialized physical therapy known as biofeedback. With biofeedback, a therapist helps to improve a person’s rectal sensation and pelvic floor muscle coordination. There are various effective techniques used in biofeedback. Some therapists train patients by teaching them to expel a small balloon placed in the rectum. Another technique uses a small probe placed in the rectum or vagina or electrodes placed on the surface of the skin around the opening to the rectum (anus) and on the abdominal wall. These instruments detect when a muscle is contracting or relaxing and provide visual feedback of the muscle action. This visual feedback helps the individual to understand the muscle movement and aids in improving muscle coordination. Approximately 75% of individuals with pelvic floor dysfunction experience significant improvement with biofeedback.
Abnormalities identified with a defecating proctogram such as rectal prolapse and rectocele may be treated with a surgical procedure.
Pilonidal Disease
What is pilonidal disease and what causes it?
Pilonidal disease is a chronic infection of the skin in the region of the buttock crease (Figure 1). The condition results from a reaction to hairs embedded in the skin, commonly occurring in the cleft between the buttocks. The disease is more common in men than women and frequently occurs between puberty and age 40. It is also common in obese people and those with thick, stiff body hair.
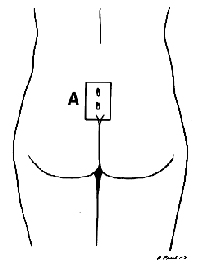
Figure 1: Pilonidal disease is a chronic skin infection in the buttock crease area. Two small openings are shown (A).
What are the symptoms?
Symptoms vary from a small dimple to a large painful mass. Often the area will drain fluid that may be clear, cloudy or bloody. With infection, the area becomes red, tender, and the drainage (pus) will have a foul odor. The infection may also cause fever, malaise, or nausea.
There are several common patterns of this disease. Nearly all patients have an episode of an acute abscess (the area is swollen, tender, and may drain pus). After the abscess resolves, either by itself or with medical assistance, many patients develop a pilonidal sinus. The sinus is a cavity below the skin surface that connects to the surface with one or more small openings or tracts. Although a few of these sinus tracts may resolve without therapy, most patients need a small operation to eliminate them.
A small number of patients develop recurrent infections and inflammation of these sinus tracts. The chronic disease causes episodes of swelling, pain, and drainage. Surgery is almost always required to resolve this condition.
How is pilonidal disease treated?
The treatment depends on the disease pattern. An acute abscess is managed with an incision and drained to release the pus, and reduce the inflammation and pain. This procedure usually can be performed in the office with local anesthesia. A chronic sinus usually will need to be excised or surgically opened.
Complex or recurrent disease must be treated surgically. Procedures vary from unroofing the sinuses to excision (Figure 2) and possible closure with flaps. Larger operations require longer healing times. If the wound is left open, it will require dressing or packing to keep it clean. Although it may take several weeks to heal, the success rate with open wounds is higher. Closure with flaps is a bigger operation that has a higher chance of infection; however, it may be required in some patients. Your surgeon will discuss these options with you and help you select the appropriate operation.
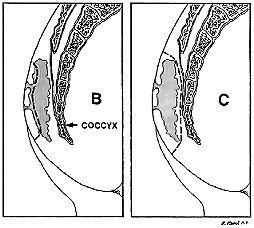
Figure 2: Drawing B is a side view showing how most of the inflammation is deep under the skin just outside the coccyx (tailbone). The dashed line shows how it may be opened or unroofed. Dashed line in drawing C shows excision of all inflamed tissue.
What care is required after surgery?
If the wound can be closed, it will need to be kept clean and dry until the skin is completely healed. If the wound must be left open, dressings or packing will be needed to help remove secretions and to allow the wound to heal from the bottom up.
After healing, the skin in the buttocks crease must be kept clean and free of hair. This is accomplished by shaving or using a hair removal agent every two or three weeks until age 30. After age 30, the hair shaft thins, becomes softer and the buttock cleft becomes less deep.
Polyps Of The Colon And Rectum
Polyps are abnormal growths rising from the lining of the large intestine (colon or rectum) and protruding into the intestinal canal (lumen). Some polyps are flat; others have a stalk.
Polyps are one of the most common conditions affecting the colon and rectum, occurring in 15 to 20 percent of the adult population. Although most polyps are benign, the relationship of certain polyps to cancer is well established.
Polyps can occur throughout the large intestine or rectum, but are more commonly found in the left colon, sigmoid colon, or rectum.
What are the symptoms of polyps?
Most polyps produce no symptoms and often are found incidentally during endoscopy or x-ray of the bowel. Some polyps, however, can produce bleeding, mucous discharge, alteration in bowel function, or in rare cases, abdominal pain.
How are polyps diagnosed?
Polyps are diagnosed either by looking at the colon lining directly (colonoscopy) or by x-ray study (barium enema).
There are three types of colorectal endoscopy: (1) rigid sigmoidoscopy, (2) flexible sigmoidoscopy and (3) colonoscopy. Rigid sigmoidoscopy permits examination of the lower six to eight inches of the large intestine. In flexible sigmoidoscopy, the lower one-fourth to one-third of the colon is examined. Neither rigid nor flexible sigmoidoscopy requires medication and can be performed in the doctor’s office.
Colonoscopy uses a longer flexible instrument and usually permits inspection of the entire colon. Bowel preparation is required, and sedation is often used.
The colon can also be indirectly examined using the barium enema x-ray technique. This examination uses a barium solution to coat the colon lining. X-rays are taken, and unsuspected polyps are frequently found.
Although checking the stool for microscopic blood is an important test for colon and rectal disorders, a negative test does NOT rule out the presence of polyps. The discovery of one polyp necessitates a complete colon inspection, since at least 30 percent of these patients will have additional polyps.
Do polyps need to be treated?
Since there is no fool-proof way of predicting whether or not a polyp is or will become malignant, total removal of all polyps is advised. The vast majority of polyps can be removed by snaring them with a wire loop passed through the instrument. Small polyps can be destroyed simply by touching them with a coagulating electrical current.
Most colon examinations using the flexible colonoscope, including polyp removal, can be performed on an outpatient basis with minimal discomfort. Large polyps may require more than one treatment for complete removal. Some polyps cannot be removed by instruments because of their size or position; surgery is then required.
Can polyps recur?
Once a polyp is completely removed, its recurrence is very unusual. However, the same factors that caused the polyp to form are still present. New polyps will develop in at least 30 percent of people who have previously had polyps. Patients should have regular exams by a physician specially trained to treat diseases of the colon and rectum.
Pruritus Ani
What is Pruritus Ani (proo-rí-tus a-ní)?
Itching around the anal area is called pruritus ani. This condition results in a compelling urge to scratch.
What causes this to happen?
Several factors may be at fault. A common cause is excessive moisture in the anal area. Moisture may be due to perspiration or a small amount of residual stool around the anal area. Pruritis ani may be a symptom of other common anal conditions such as hemorrhoids and anal fissures. The initial condition can be made worse by scratching, vigorous cleansing of the area or overuse of topical treatments.
In some individuals pruritus ani may be caused by eating certain foods, smoking and drinking alcoholic beverages, especially beer and wine. Food items that have been associated with pruritus ani include:
- Coffee, Tea
- Carbonated beverages
- Milk products
- Tomatoes and tomato products such as Ketchup
- Cheese
- Chocolate
- Nuts
Does Pruritus Ani result from lack of cleanliness?
Cleanliness is almost never a factor. However, the natural tendency once a person develops this itching is to wash the area vigorously and frequently with soap and a washcloth. This almost always makes the problem worse by damaging the skin and washing away protective natural oils.
What can be done to make this itching go away?
A careful examination by a colon and rectal surgeon or other physician may identify a definite cause for the itching. Your physician can recommend treatment to eliminate the specific problem. Treatment of pruritus ani may include these three points.
- AVOID MOISTURE in the anal area:
• Apply either a few wisps of cotton, a 4 x 4 gauze or some cornstarch powder to keep the area dry.
• Avoid all medicated, perfumed and deodorant powders. - AVOID FURTHER TRAUMA to the affected area:
• Do not use soap of any kind on the anal area.
• Do not scrub the anal area with anything – even toilet paper.
• For hygiene, it is best to rinse with warm water and pat the area dry. Use wet toilet paper, baby wipes or a wet washcloth to blot the area clean. Never rub.
• Try not to scratch the itchy area. Scratching produces more damage, which in turn makes the itching worse. For individuals that experience irresistible itching at night, wearing socks on the hands may be helpful. - USE ONLY MEDICATIONS AS DIRECTED BY YOUR PHYSICIAN. Apply prescription medications sparingly to the skin around the anal area and avoid rubbing. Prolonged use of prescribed or over the counter topical medications may result in irritation or skin dryness that can make the condition worse.
How long does this treatment usually take?
Most people experience some relief from itching within a week. If symptoms do not resolve after 6 weeks, a follow-up appointment with your colon and rectal surgeon may be needed.
Rectal Prolapse
What is rectal prolapse?
Rectal prolapse is a condition in which the rectum (the lower end of the colon, located just above the anus) becomes stretched out and protrudes out of the anus. Weakness of the anal sphincter muscle is often associated with rectal prolapse at this stage, resulting in leakage of stool or mucus. While the condition occurs in both sexes, it is much more common in women than men.
Why does it occur?
Several factors may contribute to the development of rectal prolapse. It may come from a lifelong habit of straining to have bowel movements or as a late consequence of the childbirth process. Rarely, there may be a genetic predisposition. It seems to be a part of the aging process in many patients who experience stretching of the ligaments that support the rectum inside the pelvis as well as weakening of the anal sphincter muscle. Sometimes rectal prolapse results from generalized pelvic floor dysfunction, in association with urinary incontinence and pelvic organ prolapse as well. Neurological problems, such as spinal cord transection or spinal cord disease, can also lead to prolapse. In most cases, however, no single cause is identified.
Is rectal prolapse the same as hemorrhoids?
Some of the symptoms may be the same: bleeding and/or tissue that protrudes from the rectum. Rectal prolapse, however, involves a segment of the bowel located higher up within the body, while hemorrhoids develop near the anal opening.
How is rectal prolapse diagnosed?
A physician can often diagnose this condition with a careful history and a complete anorectal examination. To demonstrate the prolapse, patients may be asked to sit on a commode and “strain” as if having a bowel movement.
Occasionally, a rectal prolapse may be “hidden” or internal, making the diagnosis more difficult. In this situation, an x-ray examination called a videodefecogram may be helpful. This examination, which takes x-ray pictures while the patient is having a bowel movement, can also assist the physician in determining whether surgery may be beneficial and which operation may be appropriate. Anorectal manometry may also be used to evaluate the function of the muscles around the rectum as they relate to having a bowel movement.
How is rectal prolapse treated?
Although constipation and straining may contribute to the development of rectal prolapse, simply correcting these problems may not improve the prolapse once it has developed. There are many different ways to surgically correct rectal prolapse.
Abdominal or rectal surgery may be suggested. An abdominal repair may be approached laparoscopically in selected patients. The decision to recommend an abdominal or rectal surgery takes into account many factors, including age, physical condition, extent of prolapse and the results of various tests.
How successful is treatment?
A great majority of patients are completely relieved of symptoms, or are significantly helped, by the appropriate procedure. Success depends on many factors, including the status of a patient’s anal sphincter muscle before surgery, whether the prolapse is internal or external, the overall condition of the patient. If the anal sphincter muscles have been weakened, either because of the rectal prolapse or for some other reason, they have the potential to regain strength after the rectal prolapse has been corrected. It may take up to a year to determine the ultimate impact of the surgery on bowel function. Chronic constipation and straining after surgical
Rectocele
What is a rectocele?
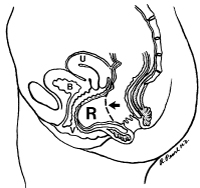 A rectocele is a bulge of the front wall of the rectum into the vagina. The rectal wall may become thinned and weak, and it may balloon out into the vagina when you push down to have a bowel movement. Most rectoceles occur in women where the front wall of the rectum is up against the back wall of the vagina. This area is called the rectovaginal septum and may be a weak area in the female anatomy. Other structures may also push into the vagina. The bladder bulging into the vagina is called a cystocele. The rectum bulging into the vagina is termed a rectocele. And the small intestines pushing down on the vagina from above may form an enterocele. Although uncommon, men may also develop a rectocele.
A rectocele is a bulge of the front wall of the rectum into the vagina. The rectal wall may become thinned and weak, and it may balloon out into the vagina when you push down to have a bowel movement. Most rectoceles occur in women where the front wall of the rectum is up against the back wall of the vagina. This area is called the rectovaginal septum and may be a weak area in the female anatomy. Other structures may also push into the vagina. The bladder bulging into the vagina is called a cystocele. The rectum bulging into the vagina is termed a rectocele. And the small intestines pushing down on the vagina from above may form an enterocele. Although uncommon, men may also develop a rectocele.
A rectocele may be present without any other abnormalities. In some cases, a rectocele may
be part of a more generalized weakness of pelvic support and may exist along with a cystocele,
urethrocele, and enterocele, or with uterine or vaginal prolapse, rectal prolapse, and fecal or
urinary incontinence.
What can cause a rectocele?
The underlying cause of a rectocele is a weakening of the pelvic support structures and thinning of the rectovaginal septum. Certain factors may increase the risk of a woman developing a rectocele. These include birth trauma such as multiple, difficult or prolonged deliveries, the use of forceps or other assisted methods of delivery, perineal tears, or an episiotomy into the rectum or anal sphincter muscles. In addition, a history of constipation and straining with bowel movements, or hysterectomy may contribute to the development of a rectocele. Commonly, these problems develop with age but they may occasionally occur in younger women or in those that have not delivered children.
What are the symptoms of a rectocele?
Many women have rectoceles but only a small percentage of women have symptoms related to the rectocele. Symptoms may be primarily vaginal or rectal. Vaginal symptoms include vaginal bulging, the sensation of a mass in the vagina, pain with intercourse or even something hanging out of the vagina that may become irritated. Vaginal bleeding is occasionally seen if the vaginal lining of the rectocele is irritated, but other sources of the bleeding should be checked by your doctor. Rectal symptoms include constipation, particularly difficult evacuation with straining. Often this is associated with bulging in the vagina when straining to have a bowel movement. Some women find that pressing against the lower back wall of the vagina or along the rim of the vagina helps to empty the rectum. At times, there will be a rapid return of the urge to have a bowel movement after leaving the bathroom because stool that was trapped in the rectocele may return to the low rectum after standing up. A general feeling of pelvic pressure or discomfort is often present but this may be due to a variety of problems.
How is a rectocele diagnosed?
Most rectoceles may be identified on a routine office examination of the vagina and rectum. However, it may be difficult to assess the size and significance of the rectocele. A more accurate method of assessing the rectocele is an x-ray study called a defecagram. This study shows how large the rectocele is and if it empties with evacuation.
When should a rectocele be treated?
You should consider having your rectocele treated when it causes significant symptoms. It takes an experienced doctor to help you decide whether your symptoms are caused by a rectocele. If there are multiple abnormalities present, it may be best to address them all at once as this will result in the best chance for improvement.
What treatment is available for a rectocele?
Rectoceles that are not causing symptoms do not need to be treated. In general, you should avoid constipation by eating a high fiber diet and drinking plenty of fluids.
Medical treatment
A bowel management program is the best first step. This includes a diet high in fiber and 6 to 8 glasses of fluids each day. Fiber acts like a sponge. It soaks up fluid so that less is removed as the stool travels around the colon. The stools will be larger, softer and easier to pass. You may wish to add a fiber supplement and/or a stool softener to this regimen to improve stool consistency. Most fiber supplements are made of psyllium, a seed product, or of a hydrophilic colloid (gel) that absorbs water. Most stool softeners are composed of docusate. This helps to smooth and lubricate the stool. Active laxatives are best avoided in most cases.
Avoid prolonged straining. If you cannot completely empty, get up and return later. Holding pressure with a finger to support the rectocele and encourage the stool to go in the correct direction is often helpful. This may be accomplished by pressing against the lower back wall of the vagina or along the posterior rim of the vagina. Avoid placing a finger inside the anus to pull the stool out as this may cause harm. A pessary may be used to support the pelvic organs. It is a ring that is inserted into the vagina and must be individually fit to each woman.
Surgical treatment
If symptoms persist even with medical therapy, then surgical repair may be indicated. There are several surgical techniques used to repair a rectocele. A rectocele repair may be performed through the anus, through the vagina, through the perineum between the anus and vagina, or from above through the abdomen. When there is extensive pelvic relaxation and prolapse, the best approach may be a combined repair.
Who should treat me for this problem?
Both colorectal surgeons and gynecologists are trained to deal with these problems. If the symptoms are entirely vaginal, then it is appropriate for your gynecologist to address the problem. If your symptoms are rectal, then a colorectal surgeon should be involved. If there is any question, seek opinions from physicians of both specialties.
Screening & Surveillance For Colorectal Cancer
What is the risk of colorectal cancer?
Colorectal cancer is the second most common cancer in the United States. The average person’s lifetime risk of developing it is about one chance in 20. The risk is increased if there is a family history of colorectal polyps or cancer, and is still higher if there is a personal history of breast, uterine or ovarian cancer. Risk is also higher for people with a history of extensive inflammatory bowel disease, such as ulcerative or Crohn’s colitis.
What is screening and surveillance?
Many polyps and cancers of the colon and rectum do not produce symptoms until they become fairly large. Screening involves one or more tests performed to identify whether a person with no symptoms has a disease or condition that may lead to colon or rectal cancer. The goal is to identify the potential for disease or the condition early when it is easier to prevent or cure. Surveillance involves testing people who have previously had colorectal cancer or are at increased risk. Because their chance of having cancer is higher, more extensive or more frequent tests are recommended.
Later in the brochure, the tests and risk groups are defined. Also, your physician can further explain the tests and their value to you.
Why should testing be undertaken?
Colorectal cancer is known as a “silent” disease, because many people do not develop symptoms, such as bleeding or abdominal pain until the cancer is difficult to cure. In fact, the possibility of curing patients after symptoms develop is only about 50%. On the other hand, if colorectal cancer is found and treated at an early stage, before symptoms develop, the opportunity to cure is 80% or better. Most colon cancers start as non cancerous growths called polyps. If the polyps are removed, then the cancer may be prevented. Major surgery can usually be avoided.
What screening tests should be done?
The simplest screening test for colon and rectal cancer is testing of the stool to detect tiny amounts of invisible blood; this is called fecal occult blood testing. This test has been available for many years, is inexpensive and very simple. Unfortunately, it only detects cancer or polyps which are bleeding at the time of the test. Only about 50% of cancers and 10% of polyps bleed enough to be detected by this test. Therefore, further screening is necessary for accurate detection of cancers and polyps.
Flexible sigmoidoscopy is a test which allows the physician to look directly at the lining of the colon and rectum. During this test, which is performed in the physician’s office, the lining of the lower one-third of the colon and rectum can usually be seen. This is the portion of the lower intestine which accounts for most polyps and cancers. When flexible sigmoidoscopy is combined with testing the stool for hidden blood, many cancers and polyps can be detected.
When a polyp or cancer is detected by flexible sigmoidoscopy, or if a person is at high risk to develop colon and rectal cancer, colonoscopy provides a safe, effective means of visually examining the full lining of the colon and rectum. Colonoscopy is used to diagnose colon and rectal problems and to perform biopsies and remove colon polyps. Most colonoscopies are done on an outpatient basis with minimal inconvenience and discomfort.
A barium enema or x-ray of the colon is almost as good as colonoscopy in detecting large tumors, but it is not as accurate for small tumors or polyps. The combination of barium enema and sigmoidoscopy is better than either test alone, but not as good as colonoscopy.
When and how often should testing be done?
For people who have none of the risks described earlier, digital rectal examination and testing of the stool for hidden blood are recommended annually beginning at age 40. Flexible sigmoidoscopy is recommended every 5 years at age 50 or older. A double contrast barium enema every 5 to 10 years, and colonoscopy every 10 years are acceptable alternatives.
Surveillance is recommended for people in the following high-risk groups:
- People who have had any pre-cancerous polyps found and removed should have colonoscopy one to three years after the first examination. Double-contrast barium enema is an alternative to colonoscopy but does not allow removal of polyps.
- People with a close relative, such as sibling, parent or child who has had colorectal cancer or a pre-cancerous polyp should have the same screening as people of average risk, but it should begin at age 40 or 5 years before the age at which the youngest was diagnosed.
- People with a family history of colorectal cancer in several close relatives and several generations, especially cancers occurring at a young age, should receive genetic counseling and consider genetic testing for a condition called hereditary nonpolyposis colorectal cancer. People with this family medical history should have an examination of the entire colon preferably colonoscopy every two years starting between the age of 20 and 30, and every year after age 40.
- People with a family history of an inherited disease called familial adenomatous polyposis (FAP) should receive counseling and consider genetic testing to see if they are carriers for the gene that causes the disease. People with this gene or whose tests are inconclusive should have a flexible sigmoidoscopy annually beginning at puberty to see if they are expressing the gene. If polyposis is present, they should discuss with their physician the need for total colectomy, which involves removing all the colon and rectum.
- People with a personal history of colorectal cancer should have a complete examination of the colon within one year after the cancer is initially detected and surgically removed. If this exam is normal, they should have a follow-up exam within three years. Examinations to evaluate the entire colon include colonoscopy or flexible sigmoidoscopy with adouble-contrast barium enema.
- People with a history of extensive inflammatory bowel disease for 8 or more years should consider having a colonoscopy examination of their colon conducted every one to two years.
- Women with a personal history of breast or female genital cancer (ovary or uterine) have a 15% lifetime risk (1 in 6) of developing colon cancer. They should undergo colonoscopy every 5 years, beginning at age 40.
Who does the screening and surveillance?
The simpler tests such as digital rectal examination, fecal occult blood testing, or flexible sigmoidoscopy may be performed by your primary care physician or your surgeon. They can also arrange for colonoscopy to be performed by a specially trained physician, such as a colon and rectal surgeon.
Ulcerative Colitis
What is ulcerative colitis?
 Ulcerative colitis is an inflammation of the lining of the large bowel (colon and rectum). Symptoms include rectal bleeding, diarrhea, abdominal cramps, weight loss, and fevers. In addition, patients who have had extensive ulcerative colitis for many years are at an increased risk to develop large bowel cancer. The cause of ulcerative colitis remains unknown.
Ulcerative colitis is an inflammation of the lining of the large bowel (colon and rectum). Symptoms include rectal bleeding, diarrhea, abdominal cramps, weight loss, and fevers. In addition, patients who have had extensive ulcerative colitis for many years are at an increased risk to develop large bowel cancer. The cause of ulcerative colitis remains unknown.
How is ulcerative colitis treated?
Initial treatment of ulcerative colitis is medical, using antibiotics and anti-inflammatory medications such as aminosalicylates. If these fail, prednisone can be used for a short period of time but long-term use can be associated with significant side effects. If prednisone is ineffective or cannot be discontinued, immunomodulators such as 6-mercaptopurine or azathioprine can be used to control active disease that does not merit hospitalization. In order to maintain control of the disease, aminosalicylates or immunomodulators are used on a long-term basis. “Flare-ups” of the disease can often be treated by increasing the dosage of medications or adding new medications. Hospitalization may be necessary to put the bowel to rest and deliver steriods directly into the blood stream.
When is surgery necessary?
Surgery is indicated for patients who have life-threatening complications of inflammatory bowel diseases, such as massive bleeding, perforation, or infection. It may also be necessary for those who have the chronic form of the disease, which fails to improve with medical therapy. It is important the patient be comfortable that all reasonable medical therapy has been attempted prior to considering surgical therapy. In addition, patients who have long-standing ulcerative colitis may be candidates for removal of the large bowel, because of the increased risk of developing cancer. More often, these patients are followed carefully with repeated colonoscopy and biopsy, and surgery is recommended only if precancerous signs are identified.
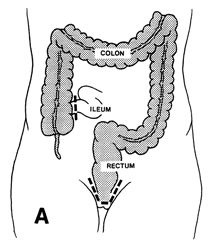 What operations are available?
What operations are available?
Historically, the standard operation for ulcerative colitis has been removal of the entire colon, rectum, and anus. This operation is called a proctocolectomy (Illustration A) and may be performed in one or more stages. It eliminates the disease and removes all risk of developing cancer in the colon or rectum. However, this operation requires creation of a Brooke ileostomy (bringing the end of the remaining bowel through the abdomen wall, Illustration B) and long-term use of an appliance on the abdominal wall to collect waste from the bowel.
The continent ileostomy (Illustration C) is similar to a Brooke ileostomy, but an internal reservoir is created. The bowel still comes through the abdominal wall, but an external appliance is not required. Instead, the internal reservoir is drained three to four times a day by inserting a tube into the reservoir. This option eliminates the risks of cancer and risks of recurrent persistent colitis, but the internal reservoir may begin to leak and require another surgical procedure to revise the reservoir.
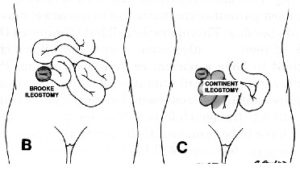
Some patients may be treated by removal of the colon, with preservation of the rectum and anus. The small bowel can then be reconnected to the rectum and continence preserved. This avoids an ileostomy, but the risks of ongoing active colitis, increased stool frequency, urgency, and cancer in the retained rectum remain.
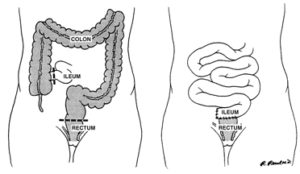
Are there other surgical alternatives?
The ileoanal procedure is the most common surgical treatment for the management of ulcerative colitis. This procedure removes all of the colon and rectum, but preserves the anal canal. The rectum is replaced with small bowel, which is refashioned to form a small pouch. Usually, a temporary ileostomy is created, but this is closed several months later. The pouch acts as a reservoir to help decrease the stool frequency. This maintains a normal route of defecation, but most patients experience five to ten bowel movements per day. This operation all but eliminates the risk of recurrent ulcerative colitis and allows the patient to have a normal route of evacuation. Patients can develop inflammation of the pouch (pouchitis), which usually responds to antibiotic treatment. In a small percentage of patients, the pouch fails to function properly and may have to be removed. If the pouch is removed, a permanent ileostomy will likely be necessary.
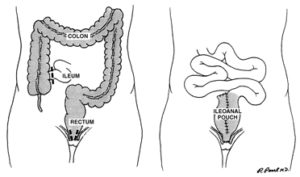
Which alternative is preferred?
It is important to recognize that none of these alternatives makes a patient with ulcerative colitis normal. Each alternative has perceivable advantages and disadvantages, which must be carefully understood by the patient prior to selecting the alternative which will allow the patient to pursue the highest quality of life.
